What Is Stress Urinary Incontinence?
Stress Urinary Incontinence (SUI) is when urine leaks unexpectedly during activities that put pressure on the bladder, such as coughing, sneezing, laughing, or exercising. The condition occurs when the pelvic floor muscles become weakened or damaged. Pelvic floor muscles are responsible for supporting the bladder and controlling the release of urine, so when they aren’t working correctly, they can’t keep urine in the bladder.
The involuntary leakage of urine associated with SUI can significantly impact your quality of life. It may cause embarrassment, social isolation, and a reduction in self-esteem. SUI can limit participation in physical activities, disrupt sleep, and affect intimate relationships.
Despite how common it is and its impact on daily life, many people with SUI do not seek medical help because they believe urinary incontinence is an inevitable part of aging. However, SUI is a treatable condition, and early diagnosis and intervention can improve symptoms and overall quality of life.
Who Gets Stress Urinary Incontinence?
SUI can affect anyone, but women are more susceptible than men. It is estimated that 15-30% of women experience SUI at some point in their lives, while the prevalence in men is around 3-11%. The chances of getting SUI increases with age and is particularly common among middle-aged and older women.
Various factors make SUI more common in women, such as pregnancy, childbirth, and menopause, which can weaken the pelvic floor muscles and tissues. Men may also develop SUI, often as a result of prostate surgery or other medical conditions that affect the urinary system.
How the Urinary System Works
The urinary system is responsible for eliminating waste, toxins, and excess water from our bodies. The kidneys continuously filter the body’s blood to remove waste and keep water and electrolytes in balance. Everything the kidneys remove is known as urine. The urine exits the kidneys, travels the down the ureters, and is stored in the bladder—a muscular sac designed to store urine until it’s time to release it voluntarily.
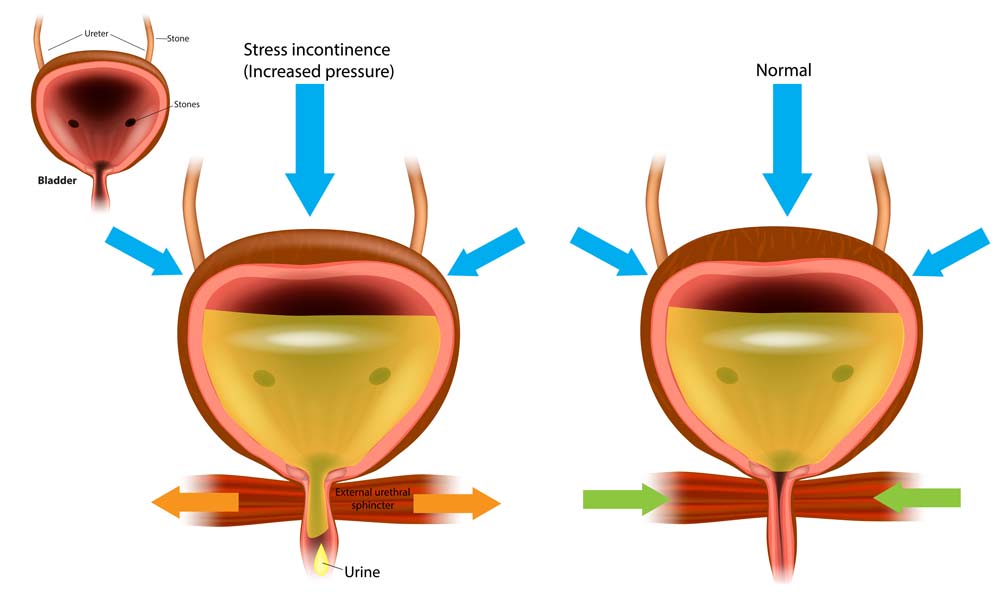
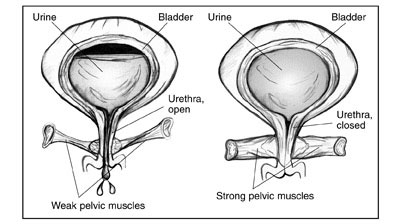
Pelvic floor muscles form a supportive sling around the bladder, urethra, and other pelvic organs. They play a critical role in keeping urine in the bladder by helping to close the urethral opening and prevent leakage.
Urinary continence is maintained through a complex interplay between the bladder, urethra, pelvic floor muscles, and the nerves that signal them. When the bladder fills with urine, the bladder muscle (detrusor) remains relaxed while the internal and external urethral sphincters contract to keep the urethral opening closed. The pelvic floor muscles also provide support and maintain closure pressure.
Normally, when it is time to urinate, the detrusor muscle contracts to push the urine out, and the urethral sphincters relax, allowing urine to flow through the urethra and exit the body. The pelvic floor muscles also relax during this process. In a healthy urinary system, these muscles and sphincters work in harmony to prevent involuntary urine leakage.
In individuals with stress urinary incontinence, the pelvic floor muscles and urethral sphincters cannot provide adequate support or maintain sufficient tone to prevent leakage during activities that put pressure on the bladder. This may be due to weakened or damaged muscles, connective tissue, or nerves.
Causes and Risk Factors for SUI
There are several reasons the pelvic floor muscles can be weakened or damaged. Here are just a few of the most common causes.
Pregnancy and Childbirth
Pregnancy and childbirth are significant risk factors for the development of SUI in women. The weight of a growing baby can exert pressure on the bladder and pelvic floor muscles, potentially causing them to weaken. Also, childbirth, especially vaginal delivery, can stretch or tear pelvic floor muscles and connective tissue, resulting in long-term damage.
The risk of developing SUI after childbirth may be influenced by factors such as the baby’s size, the use of forceps or vacuum during delivery, and the number of pregnancies a woman has had. While SUI may improve for some women in the months following childbirth, others may continue to experience symptoms.
Aging and Menopause
Aging is another risk factor for SUI, as the pelvic floor muscles and connective tissues naturally weaken over time. In women, menopause can worsen this weakening due to a decline in estrogen levels. Estrogen plays a role in maintaining the strength and elasticity of the pelvic floor muscles and tissues. As estrogen levels decrease during menopause, women may become more susceptible to developing SUI.
Obesity
Excess body weight can place additional strain on the pelvic floor muscles, increasing the risk of SUI. Studies have shown that women with a higher body mass index (BMI) are more likely to experience SUI symptoms. Weight loss, even a modest amount, can help reduce the severity of SUI and improve overall bladder function.
Other Risk Factors
Additional factors may contribute to the development of SUI, including:
- Chronic coughing: Persistent coughing, often due to smoking or lung conditions, can place repeated strain on the pelvic floor muscles and lead to SUI.
- Heavy lifting: Regularly lifting heavy objects or engaging in high-impact physical activities can weaken the pelvic floor muscles over time.
- Neurological conditions: Diseases that affect the nerves, such as multiple sclerosis or Parkinson’s disease, can interfere with the normal functioning of the bladder and pelvic floor muscles.
- Prostate surgery: In men, SUI can be a side effect of prostate surgery, particularly after a prostatectomy (removal of the prostate gland) for the treatment of prostate cancer.
Symptoms of Stress Urinary Incontinence
The primary symptom of stress urinary incontinence is the accidental leakage of urine during activities that increase pressure on the bladder like coughing, sneezing, laughing, exercising, or lifting heavy objects. The amount of urine leaked can vary from a few drops to a larger volume, depending on the severity of the condition.
Some people with SUI may also experience urge incontinence, a sudden and strong need to urinate that is difficult to control, leading to leakage. This combination of symptoms is known as mixed urinary incontinence.
Diagnosis of Stress Urinary Incontinence
The diagnostic process for SUI typically begins with a thorough medical history and physical examination. Your provider will ask about your symptoms, including their frequency and severity, and any factors that may trigger or worsen them. They will also ask about your medical history, including any past surgeries, pregnancies, or medications relevant to your condition.
During the physical examination, your healthcare provider may assess the strength of your pelvic floor muscles by asking you to contract them (a “Kegel” exercise). They may also perform a pelvic exam in women or a prostate exam in men to check for any abnormalities or other potential causes of your symptoms.
Usually, other tests will be needed to confirm the diagnosis of SUI and rule out other causes of urinary incontinence, such as:
- Urinalysis: A urine sample is tested for signs of infection, blood, or other abnormalities that may indicate an underlying condition.
- Bladder diary: You may be asked to record your fluid intake, urination frequency, and leakage episodes for a few days to help your healthcare provider better understand your symptoms.
Post Void residual (PVR) measurement: This test measures the amount of urine left in the bladder after urination, which may indicate problems with bladder emptying. - Urodynamic testing: A series of tests that measure bladder pressure, urine flow, and the function of the urethral sphincters to help determine the cause of your incontinence.
- Cystoscopy: A thin, flexible tube with a camera is inserted through the urethra to examine the bladder and urethra for abnormalities or obstructions.
Conservative Treatments for SUI
Typically, treatment for SUI will begin with the least invasive options. For many people, simple changes can provide adequate relief. If those do not work, your doctor may recommend more advanced options like surgeries.
Pelvic Floor Muscle Exercises (Kegels)
Pelvic floor muscle exercises, or Kegel exercises, are a first-line treatment for SUI. These exercises involve repeatedly contracting and relaxing the pelvic floor muscles to strengthen them, which can help improve bladder control and reduce urine leakage. Your provider or a pelvic floor therapist will provide guidance on the proper technique and recommend an exercise routine tailored to your needs.
Bladder Training
Bladder training can help improve bladder control and reduce the frequency and severity of SUI episodes. Bladder training is a behavioral therapy that aims to increase the time between urination and the amount of urine the bladder can hold. This is achieved by gradually extending the intervals between voiding and practicing urge suppression techniques.
Lifestyle Modifications
Certain lifestyle changes can help alleviate SUI symptoms and improve overall bladder health. These modifications may include:
- Maintaining a healthy weight: Weight loss can reduce the pressure on the bladder and pelvic floor muscles, decreasing SUI symptoms.
- Avoiding bladder irritants: Reducing the consumption of caffeine, alcohol, and spicy or acidic foods, which can irritate the bladder and worsen incontinence symptoms.
- Drinking adequate fluids: Ensuring proper hydration by drinking an appropriate amount of water throughout the day, but avoiding excessive fluid intake, which can overfill the bladder and exacerbate symptoms.
Pessaries and Other Devices
A pessary is a device that is inserted into the vagina to help support the bladder and urethra, thereby reducing urine leakage. They can be an effective non-surgical treatment option for SUI, particularly for women who are not candidates for surgery or prefer to avoid it. Pessaries are available in various shapes and sizes and are typically fitted by a healthcare provider.
For men, external devices such as penile clamps or compression devices may be used to apply gentle pressure to the urethra, helping to prevent urine leakage.
Surgical Treatments for SUI
Surgical treatments are typically reserved for severe cases of SUI or those who don’t respond well to conservative treatments. Your provider will help you decide which option may be best for you.
Mid-Urethral Sling Procedures
Mid-urethral sling procedures are the most common surgical treatments for SUI, particularly in women. A small, synthetic mesh sling is placed under the urethra to provide support and help keep the urethral sphincter closed during activities that increase pressure on the bladder. There are two main types of mid-urethral sling procedures: retropubic and transobturator. Both techniques have shown similar success rates in treating SUI.
Bulking Agent Injections
Bulking agent injections are when a material, such as collagen or synthetic substances, is injected into the tissues surrounding the urethra. This creates added bulk and helps to narrow the urethral opening, improving the closure mechanism and reducing urine leakage. Bulking agent injections are less invasive than sling procedures and may be an option for people who are not candidates for more extensive surgery. However, the effectiveness of bulking agents may diminish over time, and repeat injections may be required.
Other Surgical Options
There are other surgical options for SUI, although they are less commonly performed than mid-urethral sling procedures. These may include:
- Pubovaginal sling: A sling made from the patient’s tissue, donor tissue, or synthetic material is placed under the urethra to provide support. This procedure is generally reserved for cases where a mid-urethral sling has failed or is unsuitable.
- Artificial urinary sphincter: A small, inflatable cuff is implanted around the urethra, which can be manually inflated or deflated to control urine flow. This procedure is primarily used to treat SUI in men, particularly after prostate surgery.
Prevention and Management Strategies for SUI
While not all cases of SUI can be prevented, there are steps you can take to reduce your risk and maintain the health of your pelvic floor muscles and urinary system:
- Practice regular pelvic floor exercises: Kegel exercises can help strengthen the pelvic floor muscles and improve bladder control, even before SUI symptoms develop.
- Maintain a healthy weight: Achieving and maintaining a healthy weight can reduce the pressure on your bladder and pelvic floor muscles, decreasing the risk of developing SUI.
- Avoid constipation: Chronic constipation can strain the pelvic floor muscles and contribute to SUI. Eating a fiber-rich diet, drinking plenty of water, and engaging in regular physical activity can help prevent constipation.
- Avoid heavy lifting: Lifting excessively heavy objects can place too much strain on the pelvic floor muscles, increasing the risk of SUI. When lifting is necessary, use proper techniques to minimize strain on the pelvic area.
If you have been diagnosed with SUI, there are several strategies you can use to help manage your symptoms while you are finding the treatments that are most effective for you. These include:
- Use incontinence products: Absorbent pads, liners, or protective undergarments can help manage urine leakage and keep you comfortable throughout the day.
- Plan bathroom breaks: Scheduling regular bathroom breaks can help prevent bladder overfilling and reduce the likelihood of leakage.
- Limit fluid intake before bedtime: Reducing fluid intake a few hours before bedtime can help minimize nighttime incontinence and improve sleep quality.
Stress Urinary Incontinence: When to See a Doctor
For anyone experiencing the symptoms of SUI, it’s important to seek help right away. It is not something you have to live with and your provider will be able to help you find treatments that actually work.
If you’re ready to take control of your SUI and find the right treatment options for you, call today to talk to a doctor!
More Information
Questions to ask your healthcare provider when being diagnosed:
- What is causing my urine leakage problem?
- Do you think that I have SUI?
- What have my test results shown?
Questions to ask your healthcare provider about non-surgical treatment:
- What are my treatment choices, other than surgery?
- Are there any risks to vaginal inserts?
- Do you recommend one option for me over another?
- Will non-surgical treatment be enough for me?
Questions to ask about surgery:
Surgery Choices
- What are my surgery choices?
- What surgery do you recommend for me and why?
- How likely is each option going to cure or improve my leaks?
- What are the risks of sling surgery?
- How long will this treatment last?
- For slings: what type of sling material is the best choice for me and why?
- Is this surgery covered by my insurance?
- How many of these surgeries have you done, and how many do you perform yearly?
- What happens if I don’t do this surgery now?
Pre-Surgery
- Is any testing needed before surgery?
- Can you explain the test results to me?
- What kind of anesthesia will I need for this surgery?
- Should I get a second opinion? Why or why not?
Post-Surgery
- How will I feel right after my surgery? In the first week? From then on?
- What is the recovery time?
- Will I be limited in any way and for how long? Can I drive?
- When can I go back to work?
- What can I do to improve my quality of life now?