Important Message About the BCG Shortage
Bacillus Calmette-Guérin (BCG) is a standard treatment option for non-muscle invasive bladder cancer. Merck & Co., the only maker and supplier of BCG to the United States, has informed the Urology Care Foundation that they are now experiencing a global shortage of BCG due the growing use and need for this product around the world.
While Merck has raised their production of BCG, they expect this shortage to carry through 2019.
The Foundation is very concerned about this medication shortage, and we understand this situation can be stressful for physicians and patients. To help minimize disruptions to patient care, the Urology Care Foundation has been working closely with the American Urological Association (AUA), American Association of Clinical Urologists, Bladder Cancer Advocacy Network and the Society of Urologic Oncology to develop strategies to help providers treat patients with bladder cancer while this supply constraint continues.
In addition, efforts to engage the U.S. Food and Drug Administration in identifying and approving other sources of BCG are ongoing. The Urology Care Foundation remains in contact with the AUA and Merck, and will share more news as it becomes available.
For further information about BCG, please review Merck’s frequently asked questions or feel free to reach out to their National Service Center at 1-800-444-2080.
The Foundation has compiled a list of frequently asked questions regarding the BCG shortage. [pdf]
BCAN Special Update – BCG Shortage: Understanding your Treatment Options Webinar
Created February 19, 2019
Last updated March 18, 2019
What is Non-Muscle Invasive Bladder Cancer?
Bladder cancer is a type of cancer that begins in the cells lining the urinary bladder. Non-muscle invasive bladder cancer (NMIBC) is the most common subtype, accounting for approximately 75% of all bladder cancer cases. In NMIBC, cancerous cells are limited to the innermost layer of the bladder, called the urothelium or transitional epithelium, without invasion into the deeper muscle layer. If the cancer penetrates into the deeper layer of muscle, it is called muscle-invasive bladder Cancer (MIBC).
Causes
Various factors influence the development of Non-Muscle Invasive Bladder Cancer (NMIBC), although the exact cause is not always clear. Researchers have identified certain risk factors that may contribute to the development of NMIBC.
Smoking Cigarettes
Smoking is the most significant and well-established risk factor for bladder cancer of all types. Cigarette smoke contains harmful chemicals that are absorbed into the bloodstream after inhalation. The kidneys filter these chemicals and excrete them in the urine. As urine is stored in the bladder, the bladder lining is exposed to these carcinogens, increasing the risk of cellular damage and cancer development.
Occupational Exposures
Certain occupational environments can expose individuals to chemicals and substances associated with an increased risk of bladder cancer. Industries involving the production or use of chemicals like benzidine, beta-naphthylamine, and aniline dyes have been linked to a higher incidence of bladder cancer, including NMIBC. Workers in industries such as dye, rubber, leather, and printing may be at greater risk due to prolonged exposure to these carcinogens.
Age and Gender
Bladder cancer, including NMIBC, is more commonly diagnosed in older individuals, typically over the age of 40. The risk of developing bladder cancer increases with age, and most cases are diagnosed in people over 60 years old. Men are also at a higher risk of bladder cancer than women, with men being three times more likely to develop bladder cancer.
Chronic Bladder Inflammation
Chronic or recurrent bladder inflammation, such as frequent urinary tract infections or long-term use of urinary catheters, may contribute to the development of NMIBC. Inflammatory processes can cause damage to bladder cells and promote the growth of cancer in the bladder lining.
Personal and Family History
People with a personal history of bladder cancer, especially if they had NMIBC in the past, are at an increased risk of recurrence. Additionally, a family history of bladder cancer may indicate a genetic predisposition, making individuals more susceptible to NMIBC.
Arsenic in Drinking Water
In some regions, long-term exposure to high levels of arsenic in drinking water has been associated with an increased risk of bladder cancer. Arsenic is a natural element that can contaminate groundwater, posing a health risk to residents who consume the water.
Symptoms
Non-muscle invasive bladder cancer (NMIBC) can present a variety of symptoms, some of which may be subtle or easily overlooked.
Hematuria
The most common and often the initial symptom of NMIBC is hematuria, which is the presence of blood in the urine. Hematuria can present in two forms:
1. Gross Hematuria: Blood in the urine is visible, causing the urine to appear pink, red, or dark brown. Gross hematuria is more noticeable and tends to prompt immediate medical attention.
2. Microscopic Hematuria: Blood is not visible to the naked eye but can be detected through a urine test. This form of hematuria may be discovered during routine check-ups or investigations for other medical conditions.
Any episodes of hematuria, regardless of whether it is gross or microscopic, should be investigated, as it can be an early sign of bladder cancer or other urinary tract issues.
Changes in Urinary Habits
Individuals with NMIBC may experience changes in their urinary habits, which can include:
1. Increased frequency or a need to urinate more frequently than usual.
2. Urgency or a sudden and intense urge to urinate, sometimes resulting in difficulty holding urine.
3. Painful urination (dysuria) or pain and discomfort during urination. This symptom may be associated with bladder lining irritation caused by cancerous cells.
Pelvic Pain or Discomfort
Some individuals with NMIBC may experience mild to moderate pelvic pain or discomfort. This pain may be localized in the lower abdomen or pelvic region and can vary in intensity.
Lower Back Pain
In advanced cases of NMIBC, where the cancer has spread to surrounding tissues or organs, individuals may experience lower back pain. This pain may indicate the tumor has spread into nearby structures.
Symptoms of Advanced Disease
Additional symptoms may appear if NMIBC progresses to a more advanced stage or metastasizes (spreads) to distant organs. These include unexplained weight loss, fatigue, bone pain, and swelling in the legs.
Diagnosis
NMIBC is diagnosed with a series of tests. Prompt and accurate diagnosis is crucial for achieving the best possible outcomes.
Medical History and Physical Examination
The diagnostic process for NMIBC typically begins with a thorough medical history and physical examination. The physician will ask about the patient’s symptoms, risk factors, and overall health during the medical history. The physical examination may include a pelvic exam to assess the pelvic organs.
Urinalysis
One of the initial diagnostic tests for NMIBC is a urinalysis. A sample of the patient’s urine is analyzed to check for the presence of blood, abnormal cells, or signs of infection. Hematuria (blood in the urine) is a common finding in NMIBC.
Cystoscopy
Cystoscopy is used to examine the interior of the bladder. During cystoscopy, a thin, flexible tube with a camera at the end (cystoscope) is inserted through the urethra and into the bladder. The camera allows the urologist to examine the bladder walls for any abnormalities, such as tumors or areas of inflammation.
If suspicious lesions or tumors are identified during cystoscopy, the urologist may perform a biopsy to get tissue samples for further examination.
Urine Cytology
Urine cytology is another diagnostic test used in the evaluation of NMIBC. It involves examining a urine sample under a microscope to identify abnormal or cancerous cells. Urine cytology is particularly useful in detecting high-grade tumors.
However, it is essential to note that urine cytology has limitations and may not always detect low-grade tumors effectively.
Imaging Tests
Imaging tests may be conducted to assess the extent of the cancer and determine if it has spread beyond the bladder.
1. Computed Tomography (CT) Scan: CT scans can provide detailed images of the bladder and surrounding structures, helping identify tumor size, location, and potential spread.
2. Magnetic Resonance Imaging (MRI): MRI can offer high-resolution images of the bladder and nearby organs, aiding in evaluating tumor extent and invasion.
3. Ultrasonography: Ultrasound imaging may be used to examine the bladder and surrounding areas, especially in cases where a full bladder is required for other procedures.
Biopsy
A biopsy must be performed to get a final diagnosis of bladder cancer. A biopsy is a sample of tissue taken surgically that is then examined under a microscope to identify the presence of cancer cells.
Typically, a transurethral resection of bladder tumor (TURBT) will be performed using a cystoscope and special surgical instruments. If the entire tumor can be removed during the TURBT procedure, it is also considered a treatment.
Grading and Staging of Non-Muscle Invasive Bladder Cancer
Once there is a diagnosis of Non-Muscle Invasive Bladder Cancer (NMIBC), further assessments are made to determine the grade and stage of the cancer. Grading and staging are important in understanding the tumor’s aggressiveness and planning the most suitable treatment approach for each patient.
Grading of NMIBC
The grade of a cancer refers to the level of abnormality observed in the cancer cells when viewed under a microscope. The grading system most commonly used for NMIBC is the World Health Organization (WHO) grading system or the WHO/International Society of Urological Pathology (ISUP) system.
1. Low-grade (G1): Low-grade NMIBC tumors have cells that closely resemble normal bladder cells. They tend to grow slowly and are considered less aggressive.
2. High-grade (G2 and G3): High-grade NMIBC tumors exhibit more abnormal cells and rapid growth. These tumors are considered more aggressive and have a higher risk of progressing to muscle-invasive bladder cancer (MIBC).
The grade of the tumor provides valuable information about its behavior and likelihood of recurrence. Patients with low-grade tumors generally have a lower risk of recurrence than those with high-grade tumors.
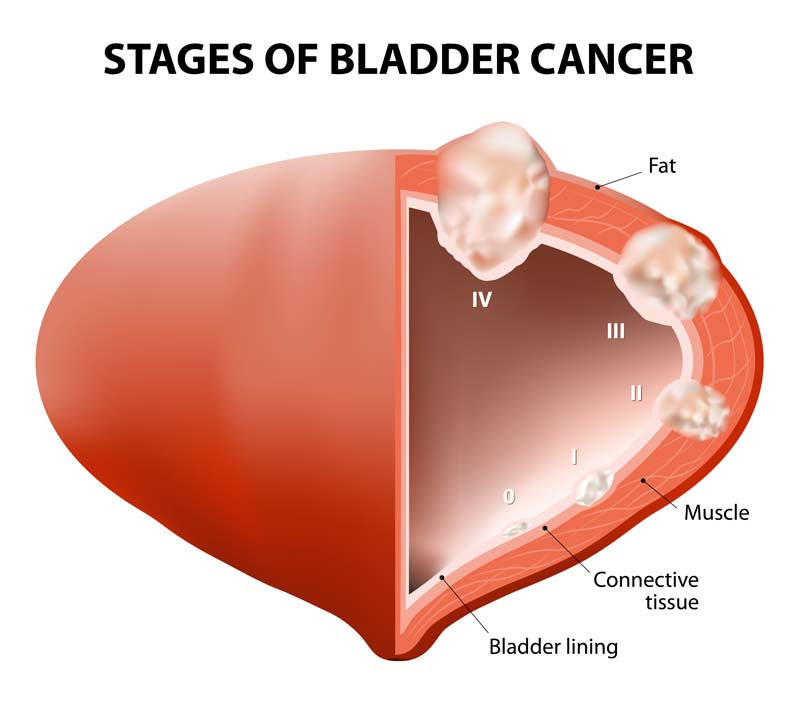
Staging of NMIBC
Staging determines the extent of cancer growth and whether it has spread beyond the original site. The staging system commonly used for NMIBC is the Tumor, Node, Metastasis (TNM) system, which takes into account three key factors:
1. T-stage (Tis, Ta, T1): The T-stage indicates the depth of tumor invasion into the bladder wall layers.
- Tis (Carcinoma in Situ): Carcinoma in situ refers to cancerous cells present only in the innermost layer of the bladder lining (urothelium). It has not invaded into deeper layers.
- Ta: In this stage, the cancer is confined to the urothelium without invading the lamina propria or deeper layers.
- T1: The tumor has invaded the lamina propria, the connective tissue layer beneath the urothelium but has not reached the muscular layer.
2. N-stage (N0): The N-stage indicates whether the cancer has spread to nearby lymph nodes. In NMIBC, the cancer has not spread to the lymph nodes.
3. M-stage (M0): The M-stage indicates whether the cancer has metastasized to distant organs. In NMIBC, the cancer has not spread to distant sites.
The combination of the T, N, and M stages provides a picture of the cancer’s extent and guides treatment decisions. Staging helps determine the most appropriate treatment approach, estimate the prognosis, and assess the risk of cancer recurrence and progression.
Treatment of Non-Muscle Invasive Bladder Cancer
NMIBC treatment is designed to remove or destroy the cancerous cells in the bladder lining while preserving bladder function. The choice of treatment depends on several factors, including the stage and grade of the cancer, the number of tumors, and the patient’s overall health. Treatment options for NMIBC include surgical procedures, intravesical therapy, and close surveillance to monitor for recurrence.
Transurethral Resection of Bladder Tumor (TURBT)
Transurethral Resection of Bladder Tumor (TURBT) is the primary treatment for most cases of NMIBC. During TURBT, a cystoscope is inserted into the bladder through the urethra. The surgeon removes the cancerous tumor(s) from the bladder lining. TURBT can both diagnose NMIBC and serve as the initial treatment.
After the tumor is removed, the tissue sample is sent to the laboratory for examination to determine the tumor grade and stage. TURBT is a minimally invasive procedure typically performed under general or spinal anesthesia.
Intravesical Therapy
Following TURBT, intravesical therapy may be recommended to reduce the risk of cancer recurrence and progression. In intravesical therapy, medication is placed directly into the bladder to target any remaining cancer cells and prevent new tumor growth.
Two common types of intravesical therapy are:
1. Immunotherapy: Bacillus Calmette-Guérin (BCG) is a weakened form of the tuberculosis bacterium. When instilled into the bladder, BCG stimulates the body’s immune system to attack and destroy cancer cells. BCG therapy is usually given as a series of treatments over several weeks.
2. Chemotherapy: Intravesical chemotherapy involves administering anticancer drugs directly into the bladder. The chemotherapy drugs target cancer cells and may help reduce the risk of recurrence. This helps limit chemotherapy’s side effects that may happen intravenously.
Surveillance and Follow-Up
After TURBT and intravesical therapy, regular surveillance is essential to monitor for tumor recurrence and ensure early detection of any new cancerous growths. Follow-up visits may include cystoscopy and urine cytology to assess the bladder lining and detect any signs of recurrence.
For low-grade, non-invasive tumors, surveillance alone may be sufficient as the risk of progression is relatively low. However, high-grade tumors or cases with a higher risk of recurrence may require ongoing intravesical therapy or other treatments.
Partial Cystecomy
In cases where the tumor is limited to a specific area of the bladder and hasn’t spread extensively, a partial cystectomy may be considered. This surgical procedure removes only the bladder portion containing the cancerous tumor while preserving the remaining healthy bladder tissue. Partial cystectomy is more conservative than radical cystectomy and aims to maintain bladder function and urinary continence. However, it is typically reserved for very localized tumors and may not be suitable for all NMIBC cases.
Radical Cystectomy
In some cases, NMIBC may resist TURBT and intravesical therapies or progress to a more advanced stage. In these situations, a more extensive surgical procedure called radical cystectomy may be recommended. Radical cystectomy involves surgically removing the entire bladder, nearby lymph nodes, and surrounding organs if the cancer has spread.
Radical cystectomy is a significant procedure that significantly impacts the patient’s quality of life, as it requires the creation of a urinary diversion to redirect urine out of the body. This procedure is generally reserved for cases of high-risk NMIBC that are unresponsive to other treatments or have advanced to a more invasive stage.
Clinical Trials: Advancing Treatment for NMIBC
Clinical trials are important in advancing medical knowledge and improving treatments for various diseases, including NMIBC. These trials involve carefully designed research studies that evaluate new therapies, treatment combinations, or diagnostic approaches.
Participating in clinical trials can provide patients with access to cutting-edge treatments and contribute to developing better therapies for NMIBC. Clinical trials may be found through a provider’s website or by visiting clincaltrials.gov.
Follow-Up Care: Monitoring and Preventing Recurrence
Following the initial treatment of Non-Muscle Invasive Bladder Cancer (NMIBC), patients require ongoing follow-up care to monitor for recurrence and manage potential side effects. Follow-up care is essential to ensure early detection of new tumors or cancer progression so they can be treated quickly for the best results.
Regular follow-up care serves several critical purposes:
1. Detecting Recurrence: NMIBC has a risk of recurrence, even after successful treatment. Regular check-ups, including cystoscopies and urine tests, allow early detection and prompt treatment of any new tumors that may develop.
2. Monitoring Progression: NMIBC may progress to a higher stage or grade for some patients. Regular monitoring helps identify any advancement in the disease, enabling timely adjustments to the treatment plan.
3. Managing Side Effects: Follow-up visits allow for discussing and managing any treatment-related side effects or complications.
Follow-Up Schedule
The follow-up schedule for NMIBC patients may vary based on individual factors, including the stage and grade of the cancer and the treatment received. Generally, follow-up care may involve:
1. Cystoscopy: Patients typically undergo cystoscopy every three to six months during the first two years after initial treatment. Depending on the results and risk of recurrence, the frequency may be reduced gradually.
2. Urine Tests: Regular urine tests are conducted to check for the presence of blood or cancer cells.
3. Imaging Tests: In some cases, imaging tests such as CT scans may be performed to assess the status of the bladder and surrounding structures.
4. Biopsies: Biopsies may be taken for further evaluation if abnormalities are detected during cystoscopy or urine tests.
5. Lifestyle Factors: Patients are often advised to adopt a healthy lifestyle, including smoking cessation and maintaining a balanced diet, to reduce the risk of recurrence.
Managing Recurrence
If NMIBC recurs during follow-up, treatment options will depend on the characteristics of the new tumors, such as their stage and grade, as well as the patient’s overall health. Treatment options may include additional transurethral resection, intravesical therapy (such as immunotherapy or chemotherapy directly into the bladder), or, in some cases, radical cystectomy (surgical removal of the bladder).
More Information
Other Helpful Muscle Invasive Bladder Cancer Resources
Bladder Cancer Advocacy Network
National Cancer Institute at the National Institutes of Health
National Library of Medicine
National Library of Medicine – Spanish Version

