What is Muscle-Invasive Bladder Cancer?
Muscle invasive bladder cancer is a type of bladder cancer that has penetrated the bladder wall’s muscle layer. The medical abbreviation is MIBC. This differs from superficial or non-muscle-invasive forms of bladder cancer, which stay in the bladder’s inner lining.
The bladder primarily serves to store urine produced by the kidneys. The bladder’s wall is structured in layers, each with a distinct function. Cancer can form in each of the layers, and when it happens in the muscle layer, it is called MIBC.
Cancer that has formed in or penetrated the muscular layer is particularly concerning because it means that the cancer has the potential to spread to other parts of the body. Its aggressive nature means that the diagnosis, treatment, and management strategies for MIBC can be more complex than non-muscle-invasive bladder cancer.
The deeper the cancer penetrates into the layers of the bladder and beyond, the greater the risk of poor outcomes and the more aggressive the treatment approach tends to be. MIBC requires prompt medical intervention to give patients the best chance of successful treatment.
Causes of Muscle-Invasive Bladder Cancer
The exact cause of MIBC is not always straightforward. Often, it is caused by a combination of genetic, environmental, and lifestyle factors. Several risk factors increase the likelihood of developing MIBC.
Smoking
One of the leading risk factors for all types of bladder cancer, including MIBC, is smoking cigarettes. The kidneys filter the harmful chemicals in tobacco and accumulate in the urine. Over time, these substances can damage the cells lining the inside of the bladder, making smoking a significant contributor to bladder cancer risk.
Occupational Hazards
Individuals exposed to certain industrial chemicals, especially those involved in producing dyes, rubber, leather, textiles, and paint products, may have an elevated risk of bladder cancer. Chemicals such as benzidine and beta-naphthylamine, previously used in the dye industry, are notable offenders.
Chronic Bladder Issues
Chronic bladder inflammation, resulting from conditions like recurrent urinary infections, bladder stones, or long-term use of urinary catheters, can enhance the risk of squamous cell bladder cancer, a subtype of bladder cancer.
Medications and Treatments
Some medications and treatments, like the chemotherapy drug cyclophosphamide or the diabetes medication pioglitazone, have been linked to bladder cancer.
Genetic and Family Factors
A family history of bladder cancer can suggest an inherited susceptibility, although most aren’t directly linked to genetic mutations. Genetic factors might increase the risk, especially when combined with external factors.
Other Contributing Factors
- Arsenic in Drinking Water: Consumption of water contaminated with arsenic can contribute to an elevated risk.
- Parasitic Infections: Particularly in certain parts of Africa and the Middle East, infections with the parasite Schistosoma haematobium can cause bladder cancer.
Evaluating Risk
While the above factors increase the risk of developing MIBC, they don’t guarantee its occurrence. And the absence of these risk factors doesn’t mean MIBC won’t grow. Regular screenings and consultations, especially for high-risk groups, are essential for early detection and intervention.
Symptoms of MIBC
Muscle-invasive bladder cancer (MIBC) symptoms may vary from person to person. Recognizing the symptoms early on is critical for timely diagnosis and intervention. While some symptoms can also indicate other less severe conditions, any persistent or recurring signs should prompt a visit to a healthcare professional.
1. Hematuria
Blood in the Urine: Often, the most noticeable symptom of bladder cancer is blood in the urine. The medical term for this is hematuria. This can manifest as urine that appears faintly pink to deep red. Sometimes, the blood might be visible only under a microscope.
2. Changes in Urinary Habits
- Frequency: A significant increase in the need to urinate without a noticeable increase in fluid intake.
- Urgency: A sudden, strong urge to urinate that might be difficult to control.
- Painful Urination: Experiencing pain or a burning sensation while urinating.
3. Advanced Symptoms
- Pain: Persistent pain in the pelvic or lower back region.
- Unintended Weight Loss: A significant drop in weight without any changes to diet or exercise routines can indicate underlying health concerns, including cancers like MIBC.
- General Fatigue: An unexplained feeling of tiredness or fatigue that doesn’t improve with rest.
Symptomatic Overlaps with Other Conditions
Many of these symptoms, especially those related to urinary habits, can also be signs of benign conditions such as urinary tract infections (UTIs), bladder stones, or an enlarged prostate in men. However, given the gravity of MIBC, it’s important to be evaluated if there are any persistent or concerning symptoms to rule out serious conditions and ensure early intervention if needed.
Diagnosis of MIBC
A prompt, accurate diagnosis of muscle-invasive bladder cancer (MIBC) is vital, as the type and stage of the cancer will guide the treatment strategy. An accurate diagnosis also aids in predicting the prognosis and potential outcomes for the patient. Diagnosis typically involves some or all of the following:
1. Initial Consultation and Physical Examination
- Medical History: A physician will begin with a thorough review of the patient’s medical history, including symptoms, risk factors, and any previous medical conditions or treatments.
- Physical Examination: The provider might conduct a physical examination, paying particular attention to the abdominal and pelvic areas to check for any irregularities or masses.
2. Cystoscopy
This procedure is performed by inserting a narrow tube (cystoscope) with a camera into the urethra, allowing the doctor to examine the inside of the urethra and bladder for tumors or abnormalities.
3. Urine Tests
- Urine Cytology: A laboratory examination of urine may be performed to check for cancer cells. The presence of abnormal cells in the urine may indicate bladder cancer. A urine cytology may be helpful in looking for the presence of other types of cells which may be present in other conditions.
- Urine Culture: This can help rule out other conditions, like urinary tract infections, which might present with similar symptoms. A urine sample is placed on a special growing medium so that bacteria, if present, can be identified.
3. Imaging Studies
- Intravenous Pyelogram (IVP): An X-ray examination where a dye is injected into a vein, and then taking X-rays as the dye travels through the kidneys, ureters, and bladder.
- Computed Tomography (CT) Scan: Provides detailed cross-sectional images of the body, which can help determine the presence, size, and location of tumors.
- Magnetic Resonance Imaging (MRI): Magnetic fields are used to produce detailed images of the body. It can be particularly useful to determine how deep the tumor is in the bladder wall.
4. Biopsy
A biopsy is the only way to get a firm diagnosis of cancer. The biopsy will confirm the presence of cancer and provide information about its grade. The most common procedure to obtain the biopsy sample is transurethral resection of bladder tumor (TURBT). A cystoscope is used to remove a sample or, if possible, the entire tumor for laboratory examination. Sometimes, TURBT is considered a treatment if all of it is removed during the procedure.
5. Further Tests for Advanced Diagnosis
If the initial tests suggest an advanced stage of cancer, additional tests like a chest X-ray, bone scan, or positron emission tomography (PET) scan might be needed to determine if the cancer has metastasized or spread beyond the bladder.
Grading and Staging of MIBC
Grading and staging are instrumental in understanding how aggressive the MIBC is and how far it has spread. These determinants influence treatment decisions and outcome predictions.
Grading: Assessing Aggressiveness
The grade of a tumor gives insight into how quickly the tumor might grow and spread. Grading is done by looking at the tumor in a microscope and comparing them to normal bladder cells.
- Low-grade tumors: These cancer cells appear somewhat similar to normal bladder cells. They typically grow more slowly and are less likely to invade deeper layers of the bladder wall or spread to other parts of the body.
- High-grade tumors: These cancer cells differ significantly from normal cells. They grow more rapidly and aggressively, with a higher likelihood of deeper invasion and spreading.
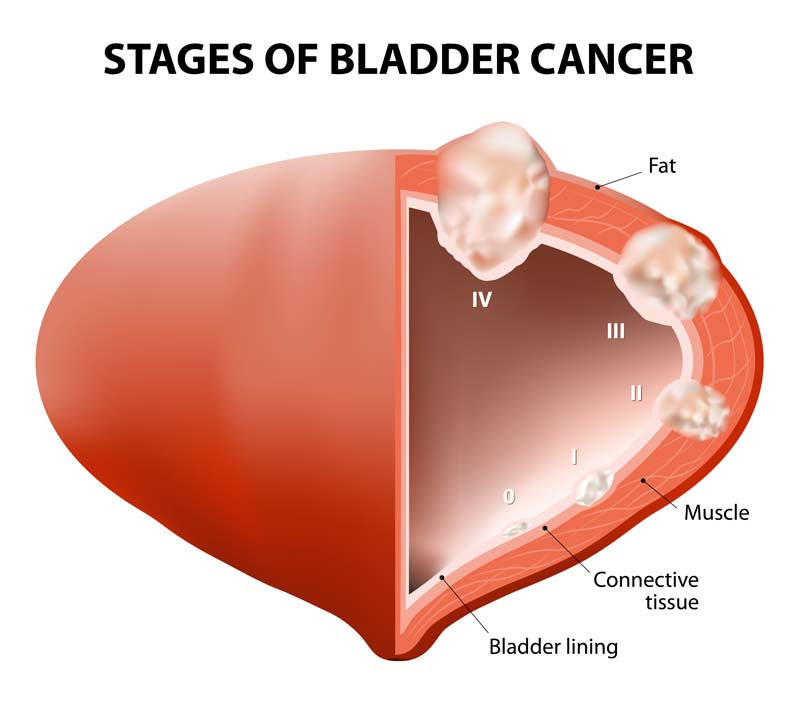
Staging: Determining the Extent
Staging describes how far cancer has spread in the body. For MIBC, it’s especially important to understand the depth of invasion into the bladder wall and beyond. Because MIBC means that the tumor has already spread into the bladder’s muscle layer, Stage I is not used to describe this type of tumor. It begins at Stage II at a minimum.
- Stage II: Here, the cancer has grown into the bladder’s muscle layer but hasn’t spread to the fatty tissue surrounding the bladder or other parts of the body.
- Stage III: The cancer has spread to the fatty tissue surrounding the bladder. It might also have grown into nearby organs like the prostate, uterus, or vagina, but hasn’t spread to the lymph nodes or distant body parts.
- Stage IV: At this advanced stage, the cancer might have spread to the abdominal or pelvic wall, nearby lymph nodes, or distant parts of the body like the bones, liver, or lungs.
Methods Used in Staging
Apart from the tests used in diagnosis, further tests might be conducted to accurately stage MIBC:
- Lymph node biopsies: To determine if cancer has spread to the lymph nodes.
- Chest X-ray: Checks for any spread to the lungs.
- Bone scans, MRI, or PET scans: Used when there’s a suspicion that the cancer has spread to other distant parts of the body.
Understanding both the grade and stage of the tumor allows for a tailored approach to treatment, ensuring the patient receives the most appropriate and effective care for their specific situation.
Prognosis
The prognosis for MIBC depends on several factors. While individual experiences can vary widely, a prognosis can help patients and their families set realistic expectations and make informed decisions about their care.
Factors Affecting Prognosis
Several elements contribute to the prognosis of MIBC:
- Stage of the Disease: The extent of tumor invasion and whether it has spread to other parts of the body is a primary factor. Cancers detected early, when they’re confined to the bladder, tend to have a better prognosis than those that have spread.
- Grade of the Tumor: High-grade tumors exhibit more cellular abnormalities, are generally more aggressive, and may carry a less favorable prognosis than low-grade tumors.
- Patient’s Overall Health: A person’s general health, age, and other underlying medical conditions can influence how well they might respond to treatment and their overall prognosis.
- Treatment Response: How the tumor responds to initial treatments, particularly surgical interventions, can provide insights into the likely disease course.
- Tumor Size and Number: Large tumors or the presence of multiple tumors can be associated with a less favorable prognosis.
Survival Rates
It’s common for patients and caregivers to seek out survival rate statistics. While these numbers can provide a broad overview, it’s essential to note that individual outcomes can differ substantially. Several factors, including advances in treatment, the patient’s overall health, and the specifics of their cancer, play into personal prognoses.
Typically, survival rates for MIBC are presented as a percentage of patients who live for a specific amount of time (often five years) after their diagnosis. These rates can vary based on the cancer’s stage at diagnosis.
For current statistics related to bladder cancer, click here.
Treatment of MIBC
The treatment approach for muscle-invasive bladder cancer (MIBC) is guided by several factors, including the tumor’s stage and grade, the patient’s overall health, age, and personal preferences. Due to the invasive nature of MIBC, treatments are often aggressive to optimize outcomes.
Surgery
- Radical Cystectomy: This is the complete removal of the bladder and is the most common treatment for MIBC. For men, this might also include the removal of the prostate and seminal vesicles, while for women, the uterus, fallopian tubes, ovaries, and part of the vagina may be removed. After the bladder is removed, surgeons will create a new way for urine to exit the body, either through an external bag or a reconstructed internal pouch.
- Segmental Cystectomy: Also known as partial cystectomy, this procedure is suitable for cases where the tumor is located in just one region of the bladder. Only the tumor and a portion of the bladder are removed.
Radiation Therapy
- External Beam Radiation Therapy (EBRT): This type of radiation uses high-energy beams directed at the tumor from outside the body. This treatment can be used as an alternative to surgery or in combination with chemotherapy, especially if surgery isn’t an option.
- Brachytherapy: Radioactive pellets or seeds are placed directly into the bladder tissue, delivering a high dose of radiation directly to the tumor while minimizing exposure to surrounding healthy tissues.
Chemotherapy
- Neoadjuvant Chemotherapy: Chemotherapy is administered before surgery to shrink the tumor, making it easier to remove and reducing the risk of cancer spreading.
- Adjuvant Chemotherapy: Given after surgery or radiation, this helps kill any remaining cancer cells, reducing the chances of recurrence.
- Systemic Chemotherapy: If the cancer has spread beyond the bladder, chemotherapy is given to target cancer cells throughout the body.
Immunotherapy
Immunotherapy enhances the body’s natural defenses to fight cancer. Bacillus Calmette-Guérin (BCG) is a type of immunotherapy for bladder cancer, where a weakened strain of tuberculosis bacteria stimulates the immune system to kill cancer cells.
Targeted Therapy
Specific drugs target particular aspects of cancer cells, inhibiting their growth and spread. While more recent, these therapies hold promise, especially when conventional treatments aren’t as effective.
Bladder Preservation Approaches
For those who wish to retain their bladder, a combination of treatments, including transurethral resection, chemotherapy, and radiation, might be employed. Regular surveillance is crucial to monitor for recurrences.
Supportive (Palliative) Care
Palliative care aims to improve the quality of life by managing pain and other symptoms. It can be used in conjunction with other aggressive treatments or when the focus shifts to comfort over cure.
Clinical Trials
Clinical trials play an essential role in advancing medical knowledge and refining treatment options for muscle-invasive bladder cancer (MIBC) and other diseases. By participating, patients can access innovative treatments that may not yet be widely available.
What Are Clinical Trials?
Clinical trials are rigorous, structured studies that test new treatments or interventions’ effects, safety, and efficacy. They can involve drugs, medical devices, surgical procedures, or other therapeutic strategies.
Phases of Clinical Trials
- Phase I: The primary aim is to evaluate the safety of a new treatment. It involves a small group of participants and looks for side effects and the appropriate dosage range.
- Phase II: This phase assesses the treatment’s efficacy and continues to monitor safety. It involves more participants than Phase I.
- Phase III: Comparing the new treatment with the current standard treatment. These trials often involve large numbers of participants across multiple locations.
- Phase IV: Post-marketing studies after a treatment has been approved and released to the public. These trials gather additional information about long-term safety and benefits.
Benefits of Participating in Clinical Trials
There are several benefits to participation in a clinical trial. These include:
- Access to new treatments: Patients have the opportunity to receive cutting-edge treatments that might be more effective than the current standard.
- Comprehensive care: Participants are closely monitored, often receiving more tests and medical attention than they would outside of the trial.
- Contribute to medical knowledge: Participation helps improve treatment strategies for future patients.
Conversely, there are risks that should be considered before participating in a trial, such as:
- Unknown side effects: As the treatment is new, there might be unforeseen side effects.
- Time-consuming: Participation often requires regular visits to the study site, additional procedures, or complex medication schedules.
- May not be beneficial: The new treatment may not be better than the current standard, or it might not work for the individual patient.
Informed Consent
Before joining a clinical trial, participants are provided with key information about the study’s purpose, procedures, potential risks, and benefits. This process ensures patients make an informed decision about their participation.
Clinical trials may be found on your provider’s website or by visiting ClinicalTrials.gov.
Follow-Up Care
Once the initial treatment phase for muscle-invasive bladder cancer (MIBC) is completed, patients transition into a phase of follow-up care. This is crucial to monitor for any signs of cancer recurrence, manage side effects from treatment, and ensure the patient’s overall well-being.
Why is Follow-Up Care Essential?
- Detect Recurrence: MIBC, like many cancers, has the potential to return. Regular check-ups can catch any recurrence early, allowing for prompt treatment.
- Manage Long-term and Late-onset Side Effects: Some side effects might persist or develop months or even years after treatment. Monitoring can identify these and initiate management strategies.
- Emotional and Psychological Support: The journey with cancer, even after treatment, can be emotionally taxing. Regular interaction with healthcare providers offers an avenue for emotional and psychological care.
Typical Follow-Up Schedule
While specific schedules vary based on individual factors and treatments received, a general outline might look like:
- First 1-2 years post-treatment: Every 3-6 months.
- Years 3-5 post-treatment: Every 6-12 months.
- After 5 years: Annually.
What to Expect During Follow-Up Visits
- Physical Examination: A thorough check to identify any new signs or symptoms.
- Lab and Imaging Tests: Depending on the treatment received, and the individual’s risk factors, various tests like blood tests, cystoscopy, CT scans, or MRIs might be scheduled.
- Discussion of Symptoms: Patients are encouraged to discuss any new or changing symptoms, as these might indicate recurrence or side effects from treatment.
- Lifestyle Counseling: Guidance on diet, physical activity, and other lifestyle factors to promote overall health and reduce cancer risk.
Side Effects and Risks of Surgery
Surgery, particularly radical cystectomy, is central to muscle-invasive bladder cancer (MIBC) treatment. Like all surgical procedures, it comes with inherent risks and potential immediate and long-term side effects.
Immediate Post-Operative Complications
- Bleeding: As with any major surgery, there’s a risk of significant blood loss during or after the procedure. Transfusions might be necessary.
- Infection: Surgical sites can become infected, requiring antibiotics and sometimes additional procedures for treatment.
- Blood Clots: Immobility after surgery can lead to the formation of blood clots in the legs, which can be life-threatening if they travel to the lungs.
- Anesthesia Reactions: Some patients might have adverse reactions to anesthesia, including allergic reactions or breathing difficulties.
Long-Term Complications
- Urinary Changes: Since the bladder is removed or altered, patients will experience changes in urinary function. A new route for urine exit, whether it’s an external bag (urostomy) or internal pouch, requires adjustment and maintenance. There’s a learning curve associated with managing these systems, and complications like stenosis, infections, or pouch stones can occur.
- Sexual Dysfunction: Men might experience erectile dysfunction or reduced sensation after the removal of the prostate and seminal vesicles. Women might face changes in sexual sensation or function due to the removal of parts of the vagina.
- Lymphedema: Swelling can occur in the legs if lymph nodes are removed, leading to fluid accumulation and lymphedema.
- Loss of Fertility: For women, the removal of reproductive organs means they can no longer bear children. Men might also face fertility issues if the prostate and seminal vesicles are removed.
Quality of Life Considerations
- Body Image Concerns: Adjusting to life with a urostomy bag or surgical scars can impact an individual’s body image and self-esteem.
- Emotional and Psychological Impact: The physical changes, coupled with the diagnosis and treatment journey, can lead to feelings of anxiety, depression, or grief.
Rehabilitation and Coping
- Physical Therapy: This can be beneficial, especially for those experiencing lymphedema or mobility issues post-surgery.
- Counseling and Support Groups: Engaging with therapists or support groups can provide emotional and psychological relief, offering coping strategies and a sense of community.
- Sexual Health Counseling: For those facing sexual dysfunction, counseling, and sometimes medication or devices, can help address and mitigate challenges.
- Education: Understanding the new urinary system, its maintenance, and potential complications empowers patients to manage their health actively.

