What is Interstitial Cystitis/Bladder Pain Syndrome?
Interstitial cystitis (IC), or bladder pain syndrome, is a chronic condition with recurring discomfort or pain in the bladder and pelvic region. If you suffer from IC, you may experience a persistent sensation of bladder pressure, reduced bladder capacity, and a need for frequent urination. The severity and duration of symptoms can differ, with some people experiencing mild symptoms while others have severe, life-disrupting discomfort.
Symptoms of Interstitial Cystitis
The symptoms of IC can vary considerably among individuals and can even change over time. Because of this, the condition can be difficult to diagnose and manage. Here are the most common symptoms of interstitial cystitis:
- Chronic pelvic pain: A persistent painful sensation in the bladder, lower abdomen, and pelvic area. The pain may be discomfort, pressure, tenderness, or intense pain.
- Increased frequency of urination: IC can cause the frequent and urgent need to urinate. In severe cases, this frequency may exceed 40 to 60 times a day, including frequent nighttime urination, known as nocturia.
- Pain during urination: Urination can be painful or cause a burning sensation.
- Pain during sexual intercourse: Discomfort or pain during sexual activities is often reported by individuals suffering from IC.
- Variation in pain: The intensity of pain may fluctuate with urinary habits, stress, menstrual cycle, or even with the consumption of certain foods or drinks.
Many of these symptoms are similar to other urological conditions, often leading to delayed diagnosis of interstitial cystitis.
Causes of Interstitial Cystitis
The exact cause of IC is unknown, making it a challenging condition to study and treat. Several theories have been proposed, suggesting that it may not be a single condition but a spectrum of disorders with similar symptoms. Here are some potential causes of IC:
- Defect in the bladder lining: One theory suggests that the bladder epithelium, a thin layer of cells that lines the bladder, is damaged. A compromised epithelium could allow substances in urine to irritate the bladder wall, leading to IC symptoms.
- Activation of mast cells: Another theory is that mast cells, which are a type of immune cell, are activated inappropriately. These cells, when activated, can release substances that promote inflammation and pain, like histamines and cytokines.
- Neurogenic inflammation: Some researchers propose that nerve growth factors are overproduced, leading to pain and inflammatory symptoms.
- Pelvic floor dysfunction: Tension or dysfunction in the pelvic floor muscles may contribute to the development of IC.
- Autoimmune response: There is evidence to suggest that, for some individuals, interstitial cystitis may be an autoimmune disorder.
- Genetic predisposition: Some research indicates a potential genetic component, as the condition seems to occur more in individuals with a family history of the syndrome.
Diagnosis of Interstitial Cystitis
Diagnosing IC can be challenging due to the variability of symptoms and the lack of a definitive test for the condition. It is often a diagnosis of exclusion, meaning other known conditions with similar symptoms must be ruled out first. Here are some steps typically taken to arrive at a diagnosis of IC:
- Medical history: A comprehensive medical history is collected to understand the patient’s symptoms, frequency, severity, and potential triggers.
- Urinalysis and urine culture: These tests help rule out urinary tract infections or other conditions with similar symptoms to interstitial cystitis.
- Bladder diary: The patient may be asked to keep a detailed diary to record the amounts of fluid intake, frequency and volume of urination, and when pain occurs.
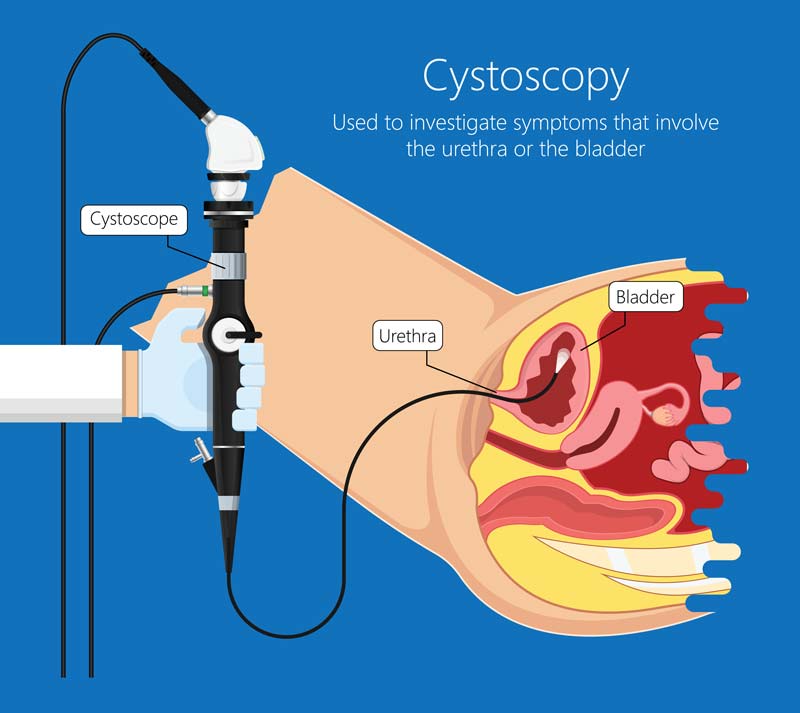
- Cystoscopy: This procedure involves inserting a thin tube with a camera (a cystoscope) into the urethra to examine the bladder and possibly perform a biopsy. Cystoscopy can help identify bladder abnormalities, such as Hunner’s ulcers, which are found in some individuals with interstitial cystitis.
- Urodynamics: This test assesses how well the bladder and urethra store and release urine. It can help identify any dysfunction in these processes.
- Potassium Sensitivity Test: In this test, water and potassium chloride are put into the bladder. Increased pain or urgency with the potassium solution, but not with water, may indicate interstitial cystitis.
While these diagnostic tools provide valuable information, no single test can definitively diagnose interstitial cystitis. A combination of tests and the physician’s clinical judgment leads to the diagnosis.
Treatment of Interstitial Cystitis
Managing interstitial cystitis is often challenging due to the variability in responses to treatment among individuals. There is currently no cure, but treatments are available to help manage symptoms. Generally, treatment consists of five steps, performed one at a time.
Step 1: Lifestyle Changes
The first step focuses on lifestyle modifications that can help to alleviate symptoms. These may include:
- Dietary changes: Certain foods and drinks are known to worsen symptoms in some individuals. Common irritants may include alcohol, caffeine, spicy foods, citrus fruits, and artificial sweeteners. Identifying and avoiding such triggers can help to manage symptoms.
- Bladder training: This involves scheduled urination times and delaying urination longer than usual to train the bladder to hold more urine and reduce frequency.
- Physical activity: Regular exercise can help reduce chronic pain symptoms and improve overall well-being.
- Stress management: Since stress can exacerbate symptoms, strategies for stress reduction, such as mindfulness, yoga, and other relaxation techniques, can be beneficial.
Step 2: Prescription Medications
If lifestyle changes are insufficient, prescription medications may be considered. These could include:
- Pentosan polysulfate sodium: The only oral medication approved by the FDA specifically for treating interstitial cystitis. This treatment is believed to protect the bladder wall.
- Antidepressants: Certain types of antidepressants can help with chronic pain.
- Antihistamines: May help to relieve urinary urgency, frequency, and other symptoms.
- Analgesics: Pain relievers may be used to manage severe pain.
Step 3: Neuromodulation Therapy, Ulcer Cauterization, and Injections
If medications are helpful, other treatments may be explored, such as:
- Neuromodulation therapy: Mild electrical pulses are used to manipulate the nerves in the lower back that influence bladder function.
Ulcer cauterization: If ulcers are present in the bladder, they can be cauterized (burned off) during a cystoscopy.
Bladder instillations: A solution containing medications is inserted directly into the bladder to reduce inflammation and pain.
Step 4: Cyclosporine
Cyclosporine is a potent immunosuppressant drug usually reserved for severe cases of interstitial cystitis that have not responded to other treatments.
Step 5: Surgery
Surgery is considered a last resort and is only used when all other treatment options have failed and quality of life is significantly impaired. Surgical options may include bladder augmentation or a complete bladder removal (cystectomy). However, these procedures have significant risks and complications, so a urologist and the patient must carefully evaluate the decision to undergo surgery.
Living with Interstitial Cystitis
While interstitial cystitis remains a challenging condition to treat, several strategies can aid in managing the symptoms and improving the quality of life.
- Self-care practices: These include following a healthy diet, maintaining regular physical activity, and getting enough rest. Self-care practices can significantly impact overall well-being and help the body better cope with chronic illness.
- Stress management: Chronic illness can be a significant source of stress, which in turn can exacerbate symptoms. Stress management techniques such as mindfulness, meditation, deep breathing, and yoga can help.
- Support networks: Connecting with others who are also dealing with IC can provide emotional support, shared coping strategies, and a sense of community. This can be achieved through online support groups, community organizations, or friends and family.
- Working with healthcare providers: Regular consultations are essential to monitor the condition, adjust treatments, and address any new or worsening symptoms. A good relationship with a healthcare provider can also provide emotional support and help individuals feel more in control of their condition.
- Psychotherapy: Dealing with chronic pain and illness can be emotionally taxing and lead to feelings of depression and anxiety. Working with a mental health professional can provide strategies to cope with these feelings and improve mental health.
- Pain management clinics: For individuals with severe pain, pain management clinics can provide specialized care and various treatment options.
- Physical therapy: For some, physical therapy targeting the pelvic floor muscles can help alleviate symptoms.
In managing interstitial cystitis, it is crucial to remember that what works best will vary from person to person. A treatment plan that may work well for one individual may not work for another. Therefore, a personalized approach, continual assessment, and adjustment of management strategies are crucial for the most effective treatment of this condition.