What is Benign Prostatic Hyperplasia (BPH)?
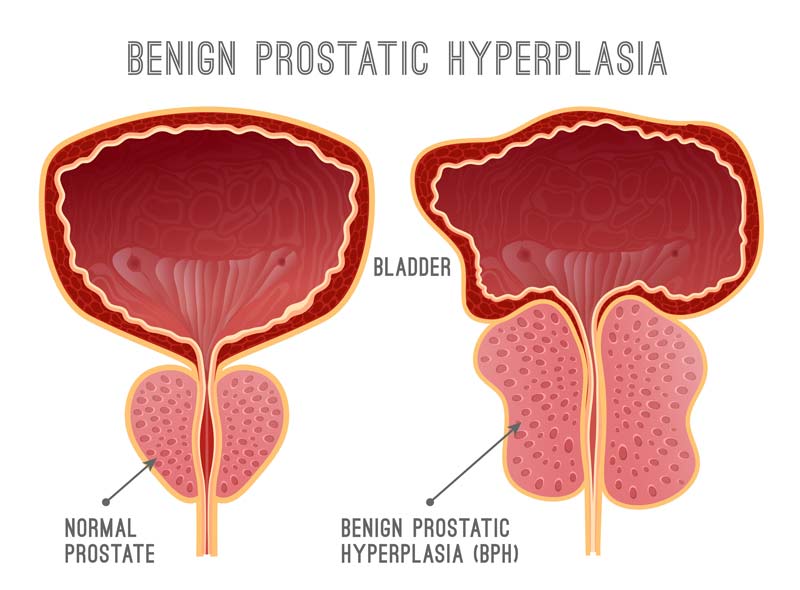
Benign Prostatic Hyperplasia, or BPH, is a condition that affects the prostate gland in men. It is characterized by an enlarged prostate, which can press against the urethra and cause problems with urination. The prostate gland typically goes through two periods of growth in a man’s life, with the second phase occurring from around age 25 until the end of a man’s life. BPH is most commonly seen during this second growth phase.
While BPH is benign and not cancerous, it is still important to seek medical attention if you are experiencing symptoms as it can sometimes occur alongside prostate cancer. BPH is also quite common, with up to 90% of men over the age of 80 experiencing it.
What is the Prostate?
The prostate is a small gland located in the male reproductive system, approximately the size of a walnut, and weighs about an ounce. It is situated below the bladder and in front of the rectum, encircling the urethra, which is the tube that carries urine from the bladder through the penis.
The primary function of the prostate is to produce fluid for semen. During ejaculation, sperm from the testicles and fluid from the prostate and seminal vesicles combine and travel through the urethra, ultimately being expelled through the penis as semen.
Symptoms
An enlarged prostate can cause problems with urination due to its pressure on the bladder. The most common symptom of BPH is frequent urination, often occurring every 1 to 2 hours, especially at night.
Other symptoms of BPH include:
- A feeling of fullness in the bladder even after urinating
- An urgent need to urinate
- A weak flow of urine
- Difficulty starting and stopping urination
- The need to strain or push to urinate.
In severe cases of BPH, a person may be unable to urinate at all, which is a medical emergency that requires immediate treatment.
How Can BPH Affect Your Life?
BPH can have a significant impact on a man’s life as it tends to worsen with age and can lead to various complications. These may include damage to the bladder and an increased risk of infection, as well as the presence of blood in the urine and potential kidney damage.
It is important to seek medical attention if you are experiencing any of these symptoms, as timely treatment can help prevent further complications.
Causes
The exact cause of BPH is not fully understood. Some researchers believe that aging and hormonal factors may play a role in its development. For example, BPH does not occur in men who have had their testicles removed before puberty.
As men age, their levels of testosterone, a male hormone, decrease while their levels of estrogen, a female hormone, increase. Some studies have suggested that the higher levels of estrogen in the prostate may contribute to the growth of prostate cells.
Another theory involves dihydrotestosterone (DHT), a male hormone that plays a role in prostate growth. Some research has shown that, even as testosterone levels decline, high levels of DHT can build up in the prostate and stimulate the growth of prostate cells. Men who do not produce DHT do not develop BPH.
Who is at Risk for BPH?
While age is the most significant risk factor for BPH, other factors may also increase a person’s risk of developing the condition.
These may include:
- Having a family history of BPH
- Being overweight or obese
- Consuming a diet high in animal fats
Can BPH be Prevented?
While it is not possible to completely prevent the development of BPH, there are steps that may help reduce the risk of developing the condition. One such measure is maintaining a healthy weight through a balanced diet that includes plenty of fruits and vegetables, as excess body fat may increase hormone levels and stimulate the growth of prostate cells.
Engaging in regular physical activity can also help control weight and hormone levels. While these steps cannot guarantee the prevention of BPH, they can contribute to overall health and well-being.
Diagnosis
If you are experiencing symptoms that may be related to BPH, or Benign Prostatic Hyperplasia, it is important to see a healthcare provider.
Seek medical attention immediately if you have blood in your urine, pain or burning while urinating, or if you are unable to urinate.
Your doctor can diagnose BPH through a combination of personal and family medical history, a physical examination, and various medical tests.
The American Urological Association (AUA) has developed a BPH Symptom Score Index, which is a series of questions that helps determine the severity of BPH symptoms.
Your doctor will review your Symptom Score and medical history, perform a physical examination, which may include a digital rectal exam, and may also recommend one or more of the following tests:
- Cystoscopy – to view the inside of the urethra and bladder
- Post-void residual volume measurement – to measure the amount of urine left after urinating
- Prostate-specific antigen (PSA) blood test – to measure markers of prostate cancer
- Ultrasound of the prostate – to look at the size and structure of the prostate
- Urinalysis – to check for signs of infection or other problems
- Uroflowmetry – to measure the speed of urine flow
- Urodynamic pressure testing – to test the bladder pressure during urination
- Urinary blood test – to screen for bladder cancer
PSA Blood Test
Prostate-specific antigen (PSA) is a protein produced exclusively by the prostate gland. In a healthy prostate, only small amounts of PSA can be detected in the blood. The PSA blood test measures the level of PSA in the bloodstream and can be conducted at a laboratory, hospital, or doctor’s office.
No special preparation is required for the test, although it is important to avoid ejaculating for 2 days prior to the test as ejaculation can temporarily increase PSA levels for 24 to 48 hours.
A low PSA level is generally considered to be a positive indicator of prostate health, while a rapid increase in PSA may indicate a problem. BPH and prostatitis, or inflammation of the prostate, are both potential causes of high PSA levels.
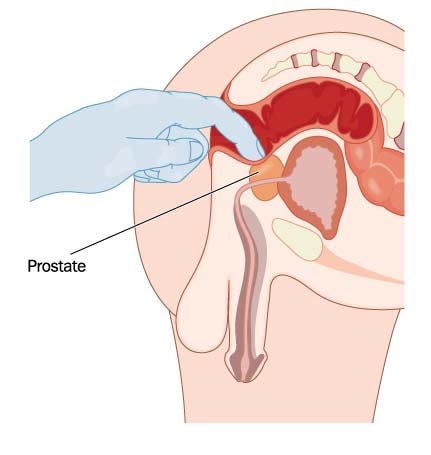
Digital Rectal Exam
A digital rectal exam (DRE) is a medical procedure in which a healthcare provider inserts a gloved and lubricated finger into the rectum to feel the prostate gland. Since the prostate is located just behind the rectum and can be accessed through the anus, a DRE is a relatively simple and non-invasive method of examining the prostate.
During the exam, the healthcare provider will feel the size, shape, and texture of the prostate to check for any abnormalities or signs of BPH, prostate cancer, or prostatitis. A DRE is generally quick and painless and can provide valuable information about the health of the prostate.
Treatment
There are a variety of treatment options available for BPH. The best course of treatment will depend on the severity of the condition and the specific needs and preferences of the patient. In some cases, a combination of treatments may be most effective.
Mild cases of BPH may not require any treatment at all.
The main types of treatment for BPH include:
- Watchful waiting / active surveillance
- Medical therapies
- Minimally invasive surgery
- Traditional surgery
Watchful Waiting/Active Surveillance
Watchful waiting, also known as active surveillance, involves closely monitoring the progression of BPH without actively treating it. This approach may involve changes to diet and the use of medication to control symptoms.
Regular check-ups with your urologist will be necessary to track the condition. If symptoms worsen or new symptoms appear, active treatment may be recommended.
The benefits of watchful waiting include the absence of side effects from medications or other treatments, but it may be more challenging to address symptoms later on. Men with mild BPH symptoms or moderate symptoms that do not significantly impact their quality of life may be good candidates for this approach.
It is important to discuss the potential risks and benefits of watchful waiting with a healthcare provider to determine if it is the right option for you.
Medical Therapies
Alpha blockers are a type of medication that can be used to treat BPH. These pills work by relaxing the muscles of the prostate and bladder, improving urine flow, and reducing blockage of the urethra. While they do not shrink the size of the prostate, they can help alleviate BPH symptoms.
Some common alpha-blocking drugs include:
- Alfuzosin (Uroxatral)
- Terazosin (Hytrin)
- Doxazosin (Cadura)
- Famsulosin (Flomax)
One benefit of alpha-blockers is that they begin to work quickly, but they may also cause side effects such as dizziness, lightheadedness, fatigue, and difficulty ejaculating.
Alpha blockers may be a good treatment option for men with moderate to severe BPH who are bothered by their symptoms, although they are not recommended for men who are preparing for cataract surgery.
5-Alpha Reducatase Inhibitors
5-alpha reductase inhibitors are another type of medication that can be helpful in treating BPH. These pills work by blocking the production of dihydrotestosterone (DHT), a male hormone that can accumulate in the prostate and stimulate its growth.
5-alpha reductase inhibitors shrink the prostate and improve urine flow, and may be taken in the form of finasteride (Proscar) or dutasteride (Avodart). These drugs can reduce the risk of complications from BPH and may also decrease the likelihood of needing surgery. However, they can cause side effects such as erectile dysfunction and reduced libido.
To maintain the benefits of treatment, it is necessary to continue taking 5-alpha reductase inhibitors. They may be most effective for men with very large prostate glands and older men.
Combination Therapy
Combination therapy involves the use of both an alpha-blocker and a 5-alpha reductase inhibitor. Studies such as the Medical Therapy of Prostatic Symptoms (MTOPS) study have shown that using two types of medication together can be more effective at improving symptoms, urine flow, and overall quality of life compared to using a single medication.
Possible combinations include finasteride (Proscar) and doxazosin (Cadura), or dutasteride (Avodart) and tamsulosin (Jalyn), which are available in a single tablet.
A urologist may also prescribe a combination of alpha-blockers and antimuscarinic drugs for patients with overactive bladder symptoms, which involve involuntary contractions of the bladder muscles and can cause urinary frequency, urgency, and incontinence.
The benefits of combination therapy include improved symptoms and the prevention of BPH progression, but it may also increase the risk of side effects. Common side effects seen in the MTOPS study included dizziness, erectile dysfunction, weakness or lack of energy, and a drop in blood pressure when standing up.
Combination therapy may be a good option for men with larger prostates.
Phytotherapies
Phytotherapy, also known as herbal treatment, is a form of self-treatment for BPH. These treatments are not prescribed by a healthcare provider and are instead purchased over the counter as dietary supplements. One popular herb used in phytotherapy is saw palmetto.
However, these treatments are not recommended by healthcare providers, as several well-designed studies have shown that they are not effective in treating BPH. Additionally, herbal treatments do not undergo the same testing and manufacturing processes as drugs, meaning that the quality and purity of over-the-counter supplements can vary.
Healthcare providers do not currently recommend the use of phytotherapies for the treatment of BPH.
Minimally Invasive Surgeries
Minimally invasive surgery is a type of surgery that is performed with minimal anesthesia and often involves a shorter recovery time. It may be performed in a doctor’s office or an outpatient center.
The type of minimally invasive surgery that is best for an individual may depend on factors such as the size of the prostate, overall health, and personal preferences.
There are several types of minimally invasive procedures available for the treatment of BPH, including:
Minimally invasive surgery can provide symptom relief and improve urinary control for some men. However, there is a risk that additional surgery may be necessary in the future.
Possible side effects of minimally invasive surgery may include:
- Urinary tract infection (UTI)
- Blood in the urine
- Burning with urination
- Increased urinary frequency
- Sudden urges to urinate
In rare cases, erectile dysfunction and retrograde ejaculation (semen flowing backward into the bladder instead of out of the penis) may also occur.
Prostate Artery Embolization (PAE) and Transurethral Needle Ablation (TUNA) are not recommended as treatments for BPH.
- Good candidates for minimally invasive surrey include men with:
- Moderate to severe BPH symptoms
- Urinary tract obstruction
- Bladder stones
- Blood in the urine
- Difficulty emptying the bladder completely
- Bleeding from the prostate
- Slow urination
- Lack of response to medications
Prostatic Urethral Lift (PUL)
Prostatic Urethral Lift (PUL), or UroLift, involves the placement of small implants in the prostate to lift and hold the enlarged gland, allowing the urethra to be unobstructed. UroLift is a quick procedure, taking only 10-15 minutes, and can often be performed in an outpatient setting.
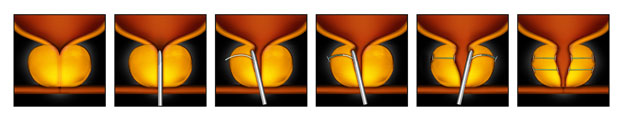
It has been FDA-approved since 2013 and has been shown to significantly improve quality of life for patients, without causing new or lasting sexual dysfunction. Some potential side effects of UroLift may include pain or burning while urinating, blood in the urine, or a strong urge to urinate, but these usually resolve within a few weeks.
Men who are allergic to certain metals should talk to their doctor before considering UroLift.
Water Vapor Therapy/ Rezum
Rezum is a minimally invasive treatment for BPH that uses steam to kill excess prostate tissue. The procedure is done in the doctor’s office with local anesthesia or after taking a pain pill, and typically takes about an hour. After the treatment, you may experience some blood in your urine and may need to use a catheter for a few days. Painful or frequent urination should improve within about 3 weeks.
Studies have shown that symptom improvement may last for up to 4 years, although it is not yet known whether the treatment continues to be effective in the long term or if additional treatment may be needed. Rezum is generally a good option for men who do not want to take medication for BPH, have tried medication and found it ineffective, or want to avoid surgery or sexual side effects. It may also be a good choice for men who have a middle lobe of the prostate or those who prefer not to have surgery.
Catheterization
Catheterization is a procedure that involves the insertion of a thin, hollow tube into the bladder to drain urine. This can be done through the urethra or through a small puncture in the bladder called a suprapubic catheter. A catheter may be temporary or indwelling, depending on the severity of the urinary blockage.
Catheterization is typically done for men who are unable to empty their bladders completely and may be used as a temporary measure until other treatments can be implemented.
There may be side effects associated with catheterization, such as irritation of the bladder or urethra, frequent urination, and burning sensation.
The main benefit of using a catheter is that it can provide temporary relief of symptoms, but there are also risks involved. The biggest risk is the potential for infection, as bacteria can accumulate on the surface of the catheter. Using a catheter for a long period of time can also increase the risk of bladder cancer and can cause irritation and tissue damage to the penis.
Men who are waiting for medication or surgery to take effect, or those with multiple medical conditions and a limited life expectancy, may be good candidates for catheterization.
Surgery
If you are experiencing severe symptoms or if medical therapy for benign prostatic hyperplasia (BPH) has failed, surgery may be necessary to remove obstructing prostate tissue. There are several types of surgery that can be performed for BPH, ranging from least to most invasive:
- Transurethral Incision of the Prostate (TUIP)
- GreenLight Laser Therapy
- Transurethral Resection of the Prostate (TURP)
- Holmium Laser Enucleation of the Prostate (HoLEP)
- Thulium Laser Enucleation of the Prostate (ThuLEP)
Transurethral Incision of the Prostate (TUIP)
Transurethral incision of the prostate (TUIP) is a surgical procedure used to treat symptoms of an enlarged prostate. It is typically used in men with smaller prostates but significant blockage of the urethra. Instead of removing prostate tissue, TUIP widens the urethra by making small cuts in the prostate and bladder neck using a laser or electrical current. This reduces pressure on the urethra and makes urination easier. The procedure is usually performed as an outpatient procedure, with a hospital stay of one to three days.
The benefits of TUIP include improved ability to urinate and reduced symptoms. However, there are also risks and potential side effects, including temporary urine retention, urinary tract infection, dry orgasm, incontinence, and erectile dysfunction. In some cases, additional treatment may be needed after TUIP.
Good candidates for TUIP include men with smaller prostates who do not want a more complete prostate resection but still need surgery. The procedure is less likely to interfere with ejaculation than more invasive surgeries, such as transurethral resection of the prostate (TURP). However, it may not be suitable for men with larger prostates or more severe symptoms.
Photoselective Vaporization (PVP)
Photoselective Vaporization of the Prostate (PVP) is also known as GreenLight Laser Therapy. During the procedure, a thin tube called a cystoscope is inserted through the urethra and into the prostate gland. The surgeon then uses a laser to vaporize or destroy excess prostate tissue that is blocking the urethra.
One of the main benefits of GreenLight is that it is done on an outpatient basis and can be performed in the hospital or doctor’s office. It is generally a safe and effective treatment for BPH, with few side effects or complications.
Many men experience significant improvement in their symptoms after GreenLight, including relief from urinary problems and improved urine flow. In addition, it does not usually cause significant blood loss and does not require a long hospital stay.
GreenLight laser therapy is typically recommended for men with small to moderate-sized prostates and those who are not suitable candidates for more invasive surgery due to other medical conditions. It is also a good option for men who want to avoid the sexual side effects associated with more invasive BPH treatments. However, it is important to note that it is not suitable for all men with BPH and that other treatment options may be more appropriate for some individuals.
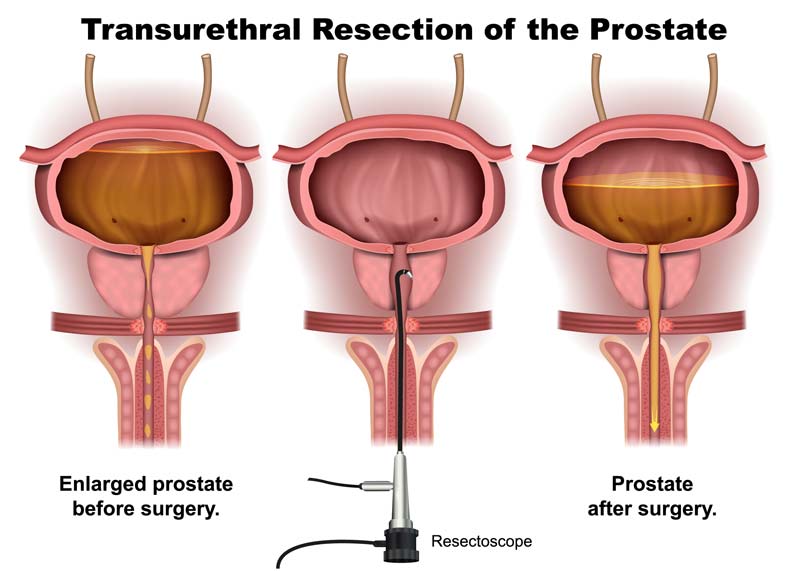
Transurethral Resection of the Prostate (TURP)
TURP is also a very common surgery for BPH. About 150,000 men in the United States have TURP each year.
After anesthesia, the surgeon inserts a thin, tube-like instrument (a resectoscope) through the tip of the penis into the urethra. The resectoscope has a light, valves for irrigating fluid, and a thin wire loop. An electrical current is passed along the wire. The surgeon uses the electrified wire to cut away prostate tissue that is blocking the urethra and seal blood vessels. The removed tissue is flushed into the bladder and from there out of the body. You will need to use a catheter for 1 to 2 days after the procedure.
What are the Benefits, Risks, and Side Effects of TURP?
Transurethral Resection of the Prostate (TURP) is a surgery that is often used to treat symptoms of BPH. During the procedure, the surgeon will insert a thin tube called a resectoscope through the urethra and into the prostate. The resectoscope has a light and a thin wire loop that is used to remove excess prostate tissue that is blocking the urethra. This procedure is typically performed under general anesthesia and requires a hospital stay of one to two days.
The benefits of TURP include long-term symptom improvement, minimal blood loss, and no incisions. However, there are also risks and side effects associated with this surgery. These may include retrograde ejaculation, erectile dysfunction, urinary tract infections, and urinary incontinence. It typically takes about four to six weeks for patients to fully recover from the procedure.
Good candidates for TURP are men who have moderate to severe BPH symptoms and require surgery.
Holmium Laser Enucleation of Prostate (HoLEP)
HoLEP is a minimally invasive procedure that involves the use of a laser to remove excess prostate tissue. The procedure is performed through the urethra using a thin, tube-like instrument called a resectoscope.
The benefits of HoLEP include rapid recovery, minimal blood loss, and a shorter hospital stay. However, like any surgery, there are risks and side effects associated with HoLEP. These may include urinary incontinence, blood in the urine, frequent or painful urination, and the risk of anesthesia.
Good candidates for HoLEP include men with larger prostates who wish to avoid more invasive surgery, and men with a higher risk of bleeding due to blood-thinning medications.
Transurethral Electroevaporation of the Prostate (TUVP)
Transurethral Electroevaporation of the Prostate (TUVP) is a less invasive alternative to more traditional surgical procedures such as TURP.
During the procedure, the surgeon inserts a resectoscope (a thin, tube-like instrument) into the urethra and uses an electrical current to destroy excess prostate tissue. The heat from the electrical current seals small blood vessels, which helps to reduce the risk of bleeding. TUVP is typically performed on an outpatient basis, and most patients are able to go home the same day without the need for a catheter.
There are several potential benefits to TUVP, including low risk of bleeding and fluid absorption, a short hospital stay (usually just one night), and the ability to return home without a catheter in most cases. However, as with any surgery, TUVP carries some risks, including the risks associated with anesthesia.
Candidates for TUVP are typically men with larger prostates who want to avoid more invasive surgery.
After Treatment
After treatment, most men experience improvement in their BPH symptoms. However, it’s possible to develop complications such as infection, bleeding, incontinence, or erectile dysfunction. In some cases, scar tissue may also form.
The long-term side effects of treatment can vary depending on the type of treatment chosen. In most cases, these side effects are temporary and may improve over time. For example, sexual function may take some time to fully return after surgery, and some men may experience retrograde ejaculation (when semen enters the bladder instead of being expelled through the penis).
To prevent a recurrence of BPH, it may be necessary to take medication to control symptoms. Some men may require additional treatment or repeated treatments to manage their symptoms. In older men, it may be possible to manage BPH symptoms effectively for the rest of their lives.
Experimental Therapies without Proven Benefit
Prostate artery embolization (PAE) is a new procedure being studied as a potential treatment for BPH. It involves injecting tiny particles into the arteries that supply blood to the prostate, which block blood flow and cause the prostate to shrink. While PAE is still being tested and its effectiveness and potential side effects are not fully known, the American Urological Association currently advises that it should only be used in clinical trials.