What is a cystoscopy?
A cystoscopy is a procedure that your doctor may use to examine your bladder to help find the cause of symptoms, or to treat or monitor conditions. This procedure allows your doctor to look directly inside your bladder and inspect the lining very closely.
If during a cystoscopy any abnormal growths or suspicious areas are seen, your doctor may remove tissue samples (biopsy) and send them to the laboratory to be examined.
A cystoscopy can be done while you are asleep under anesthesia or while you are awake with moderate sedation and/or pain management. Your doctor may instruct you to fast or have a light breakfast depending on whether you will be awake or asleep. Be sure to tell your doctor all the medications you currently take. Ask whether you should take them before your procedure or hold them until after.
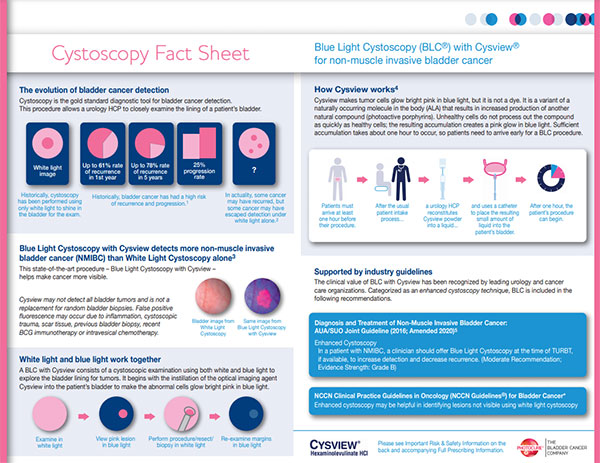
Blue Light Cystoscopy (BLC®) With Cysview® Q&A
Patients seeking treatment for bladder cancer have many choices on where to go for their care. There are more diagnostic tools and treatments now than ever before. Today, patients have an additional option when undergoing a biopsy or surgical removal (called a resection) of a suspected or known bladder cancer or for their follow-up check-up cystoscopies.1-4
BLC with Cysview is an important tool that can aid in the diagnosis and management of bladder cancer.1-4 Finding a center that offers this option can make a difference. Doctors at your institution are now using BLC with Cysview to better detect patients’ bladder cancer.
Below are the answers to some common questions about BLC with Cysview:
Q: What is BLC with Cysview?
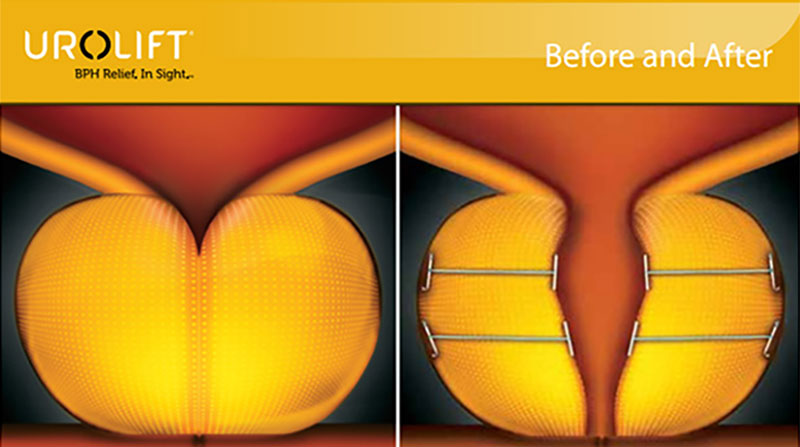
In the earliest stages of bladder cancer, cancer cells are located on the surface layer of the bladder wall. Identifying this kind of cancer, which is called non-muscle invasive bladder cancer (NMIBC), requires a correct and thorough work-up, and diagnosis is a key component of successful treatment. Understanding the stage and grade of the cancer is essential to deciding on the best treatment path.
To diagnose this disease, surgeons inspect the inside of the bladder using a long, thin tube called a cystoscope that includes a video camera on the end. In the past, the only option was white light cystoscopes, which do not always easily show tumors or cancerous lesions.
BLC with Cysview uses a cystoscope equipped with both white and blue light for visual inspection inside the bladder. A small amount (less than 2 oz.) of the prescription imaging agent Cysview is placed into the bladder using a catheter before the procedure. Together the medication and device are used to detect significantly more bladder cancer in more patients.5
Q: How is Cysview administered and how does it work?
With BLC with Cysview doctors use a cystoscope equipped with both white and blue light. Before the procedure Cysview (hexaminolevulinate HCl) is instilled into the bladder. Cysview makes the cancer cells glow bright fluorescent pink in blue light and stand out against the blue of the healthy tissue. This results in the improved detection of non-muscle invasive bladder cancer (NMIBC) lesions. Studies have found that there is a significant increase in the detection of non-muscle invasive bladder cancer.5
Q: How many patients have had BLC with Cysview?
BLC with Cysview has been used in over 450,000 patients.6 It was approved in the US in 2010 and was included in the American Urological Association (AUA) and Society of Urologic Oncology (SUO) guideline for the management of patients with non-muscle invasive bladder cancer in 2016. Over 120 centers in the US use BLC with Cysview.
Q: Does BLC with Cysview work better than white light? What are the benefits of using Cysview?
BLC with Cysview does work better than white light alone. Because Cysview causes bladder cancer cells to glow bright fluorescent pink in blue light, surgeons are better able to see smaller tumors and flat lesions that may not be seen with white light. The surgeon can immediately remove diseased tissue (called a resection), ideally leaving a clean margin of healthy tissue around the resection site. Cysview gives urologic surgeons the ability to better evaluate, identify, and remove hard-to-see tumors more accurately.1-4
By seeing more lesions, the stage and grade of the patient can be more accurately determined and appropriate management and treatment offered.
Q: Can Cysview be used as a diagnostic tool on all types of bladder cancer?
No. It is not suitable for muscle invasive bladder cancer and some patients with non-muscle invasive bladder cancer (NMIBC) after inital diagnosis and follow-up.
Bladder cancer falls into two general categories:
- Non-muscle invasive bladder cancer (NMIBC): About 70 percent of all bladder cancers fall into this category, in which a tumor (also called a lesion) is still in the inner layer of cells of the bladder’s inside wall. Subtypes include Ta, carcinoma in situ (CIS) and T1 lesions.6
- Muscle invasive bladder cancer (MIBC): This disease, which is less common than non-muscle invasive, occurs when the cancer has grown into deeper layers of the bladder wall. This disease is more likely to spread to other organs and is more difficult to treat. These cancers include the subtypes T2, T3, and T4.7
Cysview readily detects the first type, NMIBC, which may be hard to distinguish from healthy tissue. Due to their more advanced nature, MIBC tumors are detected through white light cystoscopy, biopsies, a manual exam, imaging and other diagnostic tests.1
Q: What are the limitations of BLC with Cysview?
Cysview is not a replacement for random biopsies, which still need to be done to check whether there is any disease that has not been detected under white or blue light during the cystoscopic examination. Cysview is not used for the detection of MBIC.
Q: Who is eligible for Cysview? Is Cysview right for me?
Anyone who is suspected of having or is known to have bladder cancer (from a previous cystoscopy) can have BLC with Cysview. As with all medical situations, your physician will work with you to determine if Cysview is right for your particular situation.
Q: Is Cysview with Blue Light Cystoscopy safe?
Clinical studies have shown that BLC with Cysview is safe and well-tolerated. However, no surgical procedure is free of any risk, so you should consult your doctor regarding the risks and benefits of this procedure for your individual circumstances.
Most people are ready to go home shortly after a routine procedure. Your doctor will advise you on how much rest and care you will need afterward.
References: 1. Stenzl A, Burger M, Fradet Y, Mynderse LA, Soloway MS, et al. Hexaminolevulinate guided fluorescence cystoscopy reduces recurrence in patients with nonmuscle-invasive bladder cancer. J Urol. 2010; 184(5): 1907-1913. 2. Grossman HB, Stenzl A, Fradet Y, Mynderse LA, Kriegmair M, et al. Long-term decrease in bladder cancer recurrence with hexaminolevulinate enabled fluorescence cystoscopy. J Urol. 2012; 188(1): 58-62. 3. Daneshmand S, Patel S, Lotan Y, et al. Efficacy and safety of blue light flexible cystoscopy with hexaminolevulinate in the surveillance of bladder cancer: A phase III, comparative, multicenter study. J Urol. 2018; 199(5): 1158-1165. doi: 10.1016/j. juro.2017.11.096. Epub 2017 Dec 2. 4. Daneshmand S, Bazargani ST, Bivalacqua TJ, Holzbeierlein JM, Willard B, et al. Blue light cystoscopy for the diagnosis of bladder cancer: Results from the US prospective multicenter registry. Urol Oncol. 2018. May 30. pii: S1078-1439(18)30135-2. doi: 10.1016/j.urolonc.2018.04.013. [Epub ahead of print] 5. Cysview® [prescribing Information]. Photocure, Inc. Princeton, NJ; 2018. 6. Chang SS, Boorjian SA, Chou R, Clark PE, et al. Diagnosis and Treatment of Non-Muscle Invasive Bladder Cancer: AUA/SUO Guideline. J Urol. 2016;196(4):1021-1029. 7. Pulver D, Schoenberg M, and Pulver F. Introduction to Muscle-Invasive Bladder Cancer. In Bladder Cancer: A patient-friendly guide to understanding your diagnosis and treatment options. USA: Patient-Friendly Publishing; 2017:75-76